Cost-effectiveness of revascularization strategies: the ASCERT study
- PMID:25572503
- PMCID: PMC5697906
- DOI: 10.1016/j.jacc.2014.09.078
Cost-effectiveness of revascularization strategies: the ASCERT study
Abstract
Background: ASCERT (American College of Cardiology Foundation and the Society of Thoracic Surgeons Collaboration on the Comparative Effectiveness of Revascularization Strategies) was a large observational study designed to compare the long-term effectiveness of coronary artery bypass graft (CABG) and percutaneous coronary intervention (PCI) to treat coronary artery disease (CAD) over 4 to 5 years.
Objectives: This study examined the cost-effectiveness of CABG versus PCI for stable ischemic heart disease.
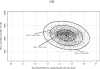
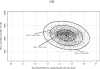
Methods: The Society of Thoracic Surgeons and American College of Cardiology Foundation databases were linked to the Centers for Medicare and Medicaid Services claims data. Costs for the index and observation period (2004 to 2008) hospitalizations were assessed by diagnosis-related group Medicare reimbursement rates; costs beyond the observation period were estimated from average Medicare participant per capita expenditure. Effectiveness was measured via mortality and life-expectancy data. Cost and effectiveness comparisons were adjusted using propensity score matching with the incremental cost-effectiveness ratio expressed as cost per quality-adjusted life-year gained.
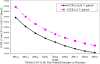
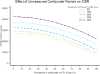
Results: CABG patients (n = 86,244) and PCI patients (n = 103,549) were at least 65 years old with 2- or 3-vessel coronary artery disease. Adjusted costs were higher for CABG for the index hospitalization, study period, and lifetime by $10,670, $8,145, and $11,575, respectively. Patients undergoing CABG gained an adjusted average of 0.2525 and 0.3801 life-years relative to PCI over the observation period and lifetime, respectively. The life-time incremental cost-effectiveness ratio of CABG compared to PCI was $30,454/QALY gained.
Conclusions: Over a period of 4 years or longer, patients undergoing CABG had better outcomes but at higher costs than those undergoing PCI.
Keywords: coronary artery bypass graft; incremental cost-effectiveness ratio; percutaneous coronary intervention; stable ischemic heart disease.
Copyright © 2015 American College of Cardiology Foundation. Published by Elsevier Inc. All rights reserved.
Conflict of interest statement
No conflict of interest
Figures




Comment in
- ASCERTing the value of coronary artery bypass graft in stable angina patients: the challenges and potential of observational research to improve care.Spertus JA.Spertus JA.J Am Coll Cardiol. 2015 Jan 6;65(1):12-14. doi: 10.1016/j.jacc.2014.10.026.J Am Coll Cardiol. 2015.PMID:25572504No abstract available.
References
- Hannan EL, Wu C, Walford G, et al. Drug-eluting stents vs, coronary-artery bypass grafting in multivessel coronary disease. N Engl J Med. 2008;358:331–41. - PubMed
- Smith PK, Califf RM, Tuttle RH, et al. Selection of surgical or percutaneous coronary intervention provides differential longevity benefit. Ann Thorac Surg. 2006;82:1420–28. discussion 1428-29. - PubMed
- Brindis RG, Fitzgerald S, Anderson HV, et al. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR): building a national clinical data repository. J Am Coll Cardiol. 2001;37:2240–5. - PubMed
- Kutcher M, Klein LW, Ou FS, et al. Percutaneous Coronary Interventions in Facilities Without Cardiac Surgery On Site: A Report From the National Cardiovascular Data Registry (NCDR) J Am Coll Cardiol. 2009;54:16–24. - PubMed
Publication types
MeSH terms
Grants and funding
LinkOut - more resources
Full Text Sources
Other Literature Sources
Medical
Miscellaneous
