economic evaluation
The story of howmy new book came to get published is long and tedious – too long and tedious to be told here in full. Let me therefore try to give you just a very brief summary:
- The ‘Apotheken Umschau‘ is a journal with a circulation of 6m in Germany.
- As it has a history of being very much pro-SCAM (so-called alternative medicine), I was surprised to be invited some 5 years ago to write a critical article about the subject.
- I was even more surprised to be invited weeks later to write a book along similar lines.
- I submitted a full book proposal and suggested the title WER RECHT HAT HEILT which is a play on words; the German dogma for SCAM practitioners is WER HEILT HAT RECHT [He who heals is right] which I turned around intoHe who is right heals. In English, this does not work very well but in German it is – I hope – quite funny.
- The proposal was swiftly accepted and I got cracking.
- When I had almost finished writing the book, I was informed that my suggested title was disallowed by the publisher’s lawyers.
- The publisher then changed the title and, as I had written the text around the agreed title, I had to rewrite much of the text.
- I nevertheless managed to meet the contractual deadline and submitted my manuscript on time.
- After a few months the first proofs arrived, and, to my surprise, the publisher had altered several crucial sections of my text. These alterations made my text less critical about SCAM.
- We then exchanged many emails and had several video conferences. Altogether I must have exchanged some 200 emails with this publisher of which about a third remained unanswered (my estimate).
- Eventually, we agreed that the publisher had the right to correct my (often rusty) German but not the content or gist of the book.
- It followed a long period of finalizing the wording of the text, the subtitles and of proofreading.
- When this was finished, I was told that the book’s publication was imminent. That was around 3 years ago.
- Looking on Amazon one day, I was struck to see my book advertised under yet another title. It had not been agreed with me. In fact, I had not even been informed about it (and hated it).
- I asked the publisher what was going on and was not given a satisfactory answer.
- Now followed a long period of silence where nothing at all happened, despite me sending increasingly angry emails from time to time.
- Then, suddenly, it was all ‘go’ again and work on the book restarted afresh.
- One day, I was told that now even my original title, ‘WER RECHT HAT HEILT’ was acceptable.
- I thus revised large sections of the book a third time.
- Now, things seemed to advance smoothly, and my book started to be advertised on numerous websites with the title page depicting ‘WER RECHT HAT HEILT’.
- But now, another surprise awaited me: I was informed that my book would need to be ‘peer-reviewed’ by two ‘experts’. I have published plenty of books and never had encountered peer-review apart from that on the initial book proposal.
- Eventually, I received the reviewers comments which were both worryingly incompetent and intensely annoying.
- I nevertheless addressed them all, if only by explaining why the reviewer was, in my view, mistaken.
- When this process was over, I was informed that the last touches were now being made on the graphics and that publication was imminent.
- However, nothing happened and my many emails asking for an explanations did not result in satisfactory explanations.
- Finally, at the end of 2024, I was informed that my book wouldnot be published. The alleged reason was that I had not adequately responded to the comments of the reviewers.
- In my view, the whole painfully long process was marked by a level of unprofessionalism on the side of the publisher that, in my extensive experience as an author, I had never encountered before.
- Luckily, the copyright was returned to me.
- Now I was free to contact another publisher, the ALIBRI VERLAG, and they accepted to publish my book.
- I then revised and updated my text yet again and, within just 4 months, my book finally saw the light of day.

In retrospect, I quite understand that publishers who are into promoting SCAM and heavily rely on advertising cannot afford to publish a book criticising SCAM. This would, of course, be bad for business! What I don’t get, however, is
why ask me and accept my book outline in the first place?
PS
As the book is in German, I will soon post a translation of a short section that explains what it is all about.
Share this:
I recently asked ‘GOOGLE GEMINI’ about my problems with King Charles. The reply was concise, to the point and roughly correct:
Edzard Ernst’s “problem” with King Charles (then Prince Charles) stemmed from a fundamental disagreement over the promotion and integration of complementary and alternative medicine (CAM) within mainstream healthcare, particularly the National Health Service (NHS) in the UK.
Here’s a breakdown of the key issues:
- King Charles’s Advocacy for CAM: King Charles has been a long-time, vocal proponent of various alternative therapies, including homeopathy, and has actively lobbied for their greater inclusion in the NHS.He established and supported organizations like The Prince’s Foundation for Integrated Health to promote these views.
- Ernst’s Evidence-Based Approach: Edzard Ernst, as the world’s first professor of complementary medicine, took a strictly evidence-based approach.His research consistently aimed to evaluate the efficacy and safety of CAM treatments through rigorous scientific methods (like systematic reviews and meta-analyses).He concluded that the vast majority of alternative therapies lacked scientific evidence of effectiveness beyond a placebo, and some were even potentially harmful.
- Clash over the Smallwood Report (2005): A major point of contention was a report commissioned by Prince Charles in 2005, written by economist Christopher Smallwood, which claimed CAM was cost-effective and should be available on the NHS.Ernst was initially involved in this report but withdrew his name and publicly denounced it as “complete misleading rubbish,” stating that the conclusions were written before the evidence was properly reviewed.He argued the report failed to address whether CAM treatments were actually effective.
- Lobbying and “Black Spider Letters”: Ernst criticized King Charles for “relentlessly meddling” in UK health politics and for using his influence to push for unproven treatments. This included Charles’s infamous “black spider letters” (so-called due to his distinctive handwriting) to government officials, lobbying for the inclusion of alternative therapies, such as homeopathy, in the NHS.
- “Duchy Originals” Products: Ernst also criticized products sold by Duchy Originals (a company founded by Prince Charles) that made unproven health claims, such as “Detox Tincture,” calling them “outright quackery” and “financially exploiting the vulnerable.”
- Impact on Ernst’s Career: The dispute had personal repercussions for Ernst.Prince Charles’s private secretary, Sir Michael Peat, filed a complaint with Exeter University, alleging that Ernst had breached confidentiality regarding the Smallwood report. Although Ernst was eventually “cleared of wrongdoing,” he stated that the ensuing 13-month university investigation was “very unpleasant” and led to the cessation of funding for his research unit, ultimately contributing to his early retirement. He felt that the university, despite clearing him, treated him as “persona non grata.”
In essence, the “problem” was a clash between the King’s personal conviction and advocacy for alternative medicine, and Ernst’s unwavering commitment to scientific rigor and evidence-based healthcare.Ernst believed that the King’s promotion of unproven therapies was irresponsible, potentially harmful to public health, and undermined scientific progress in medicine.
______________________
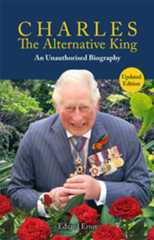
In case you want to learn the full details about “the King’s personal conviction and advocacy for alternative medicine”, please read the book below.
Share this:
Common Harms of CSM
- Musculoskeletal discomfort: Temporary soreness, stiffness, or pain in the muscles or joints after treatment.
- Headaches: Some individuals may experience headaches following spinal manipulation.
- Fatigue: Feeling tired or experiencing fatigue after treatment.
These harms occur after CSM in about 50% of all patients. They impact on their quality of life and usually last 1-3 days.
Serious Harms of CSM
- Vertebral artery dissection (VAD) and stroke: A tear in the vertebral artery can lead to stroke; the harm can be permanent.
- Death: A stroke can be fatal.
- Atlantoaxial dislocation
- Spinal cord injury: Damage to the spinal cord, potentially resulting in numbness, weakness, or paralysis.
- Herniated discs: Manipulation can exacerbate existing disc issues or cause a new disc herniation.
- Fractures: Osteoporotic patients or those with bone conditions are at risk of vertebral fractures.
- Cauda equina syndrome: Compression of nerves in the lower spine, potentially causing bowel or bladder dysfunction.
- Nerve damage: Injury to spinal nerves, leading to numbness, tingling, or weakness.
- Eye Injuries: these include central retinal artery occlusion, nystagmus, Wallenberg syndrome, ptosis, loss of vision, ophthalmoplegia, dipiopia and Horner’s syndrome.
The frequency of these harms is not known.
Other Risks
- Neglect: This happens whenever a chiropractor treats a condition that can more effectively be treated with another therapy.
- Misleading advice: This occurs whenever a chiropractor gives advice outside his area of competence, for instance, a recommendation against immunisations.
- False diagnoses: Chiropractors often diagnose a ‘vertebral subluxation’, a condition that exists only in their fantasy.
- Worsening of existing conditions: Manipulation may exacerbate underlying spinal problems or conditions like spinal instability.
- Waste of money: This occurs each time a patient pays for ineffective CSM.
The frequency of these risks is not well-documented but can be estimated to be very high.
_____________________________
I have often pointed out that the value of a therapy is not solely determined by its potential for harm. It depends crucially on the risk/benefit profile. The benefits of CSM are few and mostly uncertain. Thus the question arises:
DO THE BENEFITS OF CSM OUTWEIGH ITS RISKS?
I let you, the reader, answer this question.
PS
References for the above statements can be found inmy book.
Share this:
Donald Trump has recently made a range of nominations/appointments in the US health sector. They will influence conventional and so-called alternative medicine (SCAM) in the US and beyond. It therefore reasonable to look at the backgrounds and qualifications of these men and women and evaluate their suitability for these leadership roles.
In part 1 of this series, I discussed Robert F Kennedy Jr. and Dave Weldon; inpart 2, we evaluated Janette Nesheiwat and Casey Means; in part 3, I looked at Marty Makary and Mehmet Oz. In the 4th and last part of the series, I discuss Jay Bhattacharya and Gustav Chiarello.
Jay Bhattacharya – Director of National Institutes of Health (NIH)
Jay Bhattacharya is a physician and health economist. He also is a critic of Fauci and a co-author of the infamous Great Barrington Declaration (2020), which advocated for “herd immunity” over lockdowns during the COVID-19 pandemic. His new role would involve overseeing the NIH’s $48 billion budget. According to Kennedy’s plan, he would redirect much of the NIH funding toward alternative health approaches.
As Bhattacharya has not managed large research institutions, his ability to lead NIH effectively might be limited. His economic perspective could prioritize cost-effective research, and his opposition to lockdowns may appeal to those skeptical of them.
In summary, Bhattacharya’s academic credentials make him a fairly reasonable choice for NIH director, but his unreasonable pandemic views and lack of large-scale administrative experience raise concerns about his ability to lead the NIH effectively and without major disruptions.
Gustav Chiarello – Assistant Secretary for Financial Resources (HHS)
Gustav Chiarello has degrees in economics, public policy, and law. He is/was the Senior Special Counsel to the House Judiciary Committee, former attorney at the Federal Trade Commission (FTC), and advisor to FTC Acting Chairman Maureen Ohlhausen during Trump’s first term. He has legal and policy experience as well as skills for overseeing HHS financial resources. However, his limited healthcare-specific experience may hinder his ability to address complex HHS budgeting challenges.
In summary, Chiarello appears competent for the new role. However, his lack of healthcare expertise may prove to be a drawback.
Context and concerns
A recurring theme across the mentioned nominees and appointments is their stance against vaccinations or public health mandates. This is already eroding trust in immunization programs, increasing infection rates and creating risks to public health. Another common concern is the lack experience of most individuals in managing large bureaucracies. This is likely lead to inefficiencies or mismanagement in crucial healthcare agencies.
The nominees/appointments will drive deregulation, reduce Medicaid funding and shift NIH research priorities toward alternative health. These changes are unlikely to generate improvements in US public health. Policies driven by misinformation or ideological agendas will lead to increased uninsured rates, reduced research funding, and public health setbacks.
The group’s competence is undermined by a pattern of vaccine skepticism, promotion of pseudoscience and limited administrative experience. The risks of disrupting scientific research, immunization programs, and healthcare access are real and substantial.
Because my expertise and understanding is limited to medicine, my discussions were confinded to the realm of healthcare. But Trump appointed people in all areas, of course. My limited expertise tells me that some of these have been even more disasterous than the ones we evaluated here. I have little doubt that Trump is about to change the world – and I fear that this will not be to the better.
Share this:
The French newspaper ‘L’Express’ just published anopen letter that might be of considerable relevance to the readers of this blog. Here is my translation:
Since 2016, all private sector employers have been required by law to offer supplementary health insurance to their employees. As a result, 96% of the population is now covered. The costs for this are also borne by each household, social security contributions and common taxes used to fund the general health insurance scheme.The same obligation applies since 2020 for the State in respect of its civil servants, and the French Ministry of Education, the country’s largest public employer, has just signed contracts with MGEN and CNP assurance. This contract, which complies with the ministerial order implementing the law and setting out the cover provided, is a cause for concern, as it provides for coverage of non-conventional healthcare practices (e.g. homeopathy, osteopathy, acupuncture, naturopathy, chiropractic, relaxation therapy, etc.). According to the Ministry of Health itself, most of these practices have ‘not been the subject of scientific or clinical studies demonstrating their modes of action, their effects, their effectiveness or their harmlessness’.This coverage would reinforce the general public’s belief that these treatments are effective. This is happening while proven therapies such as psychology, prescription sport and dietetics are rarely covered by mutual insurance companies.In a report published in September 2024, the French Senate proposed to counter the sharp rise in complementary health insurance charges by reviewing the coverage of unconventional healthcare practices (so-called alternative medicine, SCAM). According to this report, the cost of these practices has increased fivefold over the last eight years, reaching almost €1 billion in 2023, excluding the cost of spa treatments.
Therapeutic excesses
We support this proposal. It is clear to us that, in addition to being useless, these unproven practices mislead patients as to what constitutes genuinely effective treatments, when in fact they are nothing more than an expenditure that does nothing to improve the health of anyone, at the expense of genuinely beneficial care. What’s more, they expose us to the risk of therapeutic aberrations, or even the abandonment of care in cases where it is necessary.The government says it wants to make savings on health spending. Wouldn’t it be more effective, and also better understood by the general public, to do so by promoting treatments whose effectiveness is supported by a scientific consensus? And would it not be better to stop the reimbursement of unproven practices likely to lead to delays in treatment and health abuses? We need to set a limit on ‘private solidarity’ expenditure, the cost of which continues to rise well above the rate of inflation, particularly for the most vulnerable households and the elderly.
The Ministry’s announcement of initiatives to combat misinformation in the health sector cannot be reconciled with the funding of unconventional therapies, about which Miviludes has repeatedly warned. The work of the Descartes Foundation shows that sensitivity to these practices and sensitivity to esotericism are linked, creating a breeding ground for health misinformation and conspiracy theories.
An individual choice
Mutual insurance companies cannot legitimise wellness practices at the expense of optimum reimbursement for proven treatments. Health issues are everybody’s business, and the most vulnerable should be able to count on national solidarity in the interests of all French people.
The CollectifNo FakeMed is calling on the authorities to be rigorous in ensuring that only practices based on scientific knowledge, in both health economics and evidence-based medicine, are covered by the public purse and mutual insurance companies. It is possible to offer a cover for some wellness treatments, but this must be a matter of personal CHOICE, and therefore an option, not an obligation.
Signatories
Institutions and associations:
- Collectif No Fakemed;
- Conseil national de l’ordre des masseurs-kinésithérapeutes;
- Conseil national de l’Ordre des Sages Femmes;
- Conseil national de l’Ordre des pédicures-podologues;
- Collectif ‘Vaccins France informations & discussions’;
- Collectif Chanology France; syndicat ReAGJIR.
Individual signatories:
- Pr Agnès Buzyn, ancienne ministre, présidente du think tank Evidences ;
- Dr Pierre de Bremond d’Ars, médecin généraliste et président du Collectif No Fakemed ;
- Isabelle Derringer, présidente du Conseil de l’Ordre des Sages Femmes ;
- Pascale Mathieu, présidente du Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Dr Eric May, médecin généraliste, directeur santé Malakoff, président de la Fédération Nationale de Formation des Centres de Santé ;
- Éric Prou, président de l’Ordre national des pédicures podologues ;
- Dr Sophie Augros, médecin généraliste ;
- Dr Mehdi Bahaji, anesthésiste-réanimateur ;
- Marie-Ange Barbier, diététicienne, membre du bureau du collectif No Fakemed ;
- Dr Damien Barraud, médecin hospitalier ;
- Karine Brezellec, trésorière adjointe du Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Dr Laurent Brindel, membre du bureau du collectif No Fakemed ;
- Gérald Bronner, professeur à la Sorbonne, membre de l’Académie nationale de médecine, membre de l’Académie des technologies ;
- Dr Matthieu Calafiore, Maître de conférences des universités, directeur du département de médecine générale de l’Université de Lille ;
- Dr Julie Chastang, médecin généraliste, maîtresse de conférence des universités (Sorbonne Université) ;
- Pr Laurence Compagnon, médecin généraliste ;
- Dominique Costagliola, membre de l’Académie des sciences, directrice de recherche émérite Inserm ;
- Laurent Cordonier, docteur en sciences sociales, Chercheur associé au GEMASS, Sorbonne Université – CNRS (UMR 8598) ;
- Dr Raphaël Dachicourt, président de Réagir ;
- Dr Jeremy Descoux, Cardiologue, Président fondateur du Collectif No Fakemed ;
- Arthur Dian, ancien ostéopathe, M2 en histoire et philosophie des sciences ;
- Jean-François Dumas, secrétaire général du Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Pr Edzard Ernst, MD, PhD, FMEdSci, FRSB, FRCP, FRCP(Edin.) professeur émérite à l’Université d’Exeter;
- Élisabeth Feytit, créatrice du podcast d’éducation à l’esprit critique Méta de Choc ;
- Dr Jean-Jacques Fraslin, médecin généraliste ;
- Roger-Philipe Gachet, Secrétaire Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Dr Julien Gere, neurologue ; Pr André Grimaldi, diabétologue ;
- Florian Gouthière, journaliste scientifique ;
- Dr Nicolas Groëll, médecin généraliste ;
- Dr Jérome Grosjean, biologiste ;
- Kalou, créateur de contenu dédié à l’information et la prévention du phénomène sectaire ;
- Jean-Paul Krivine, rédacteur en chef de Science et pseudo-sciences, Association française pour l’information scientifique ;
- Dr Corentin Lacroix, Whydoc, médecin généraliste et vulgarisateur ;
- Marion Lagneau, trésorière du collectif No Fakemed ;
- Guillaume Limousin, ingénieur, docteur en sciences, professeur de mathématiques en collège ;
- Dr Christian Lehmann, médecin généraliste et écrivain ;
- Dr Stéphanie Marsan, médecin généraliste, membre du bureau du collectif No Fakemed ; Dr Elodie Lemarthe, secrétaire générale du collectif No Fakemed ;
- Dr François Maignen, docteur en pharmacie et statisticien ;
- Dr Hervé Maisonneuve, médecine de santé publique ;
- Gilles Marchiano, secrétaire adjoint du Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Pr Matthieu Molimard, professeur de pharmacologie CHU de Bordeaux ;
- Dr François Morel, chirurgien, membre du bureau du collectif No Fakemed ;
- Dr Nathan Peiffer Smadja, infectiologue ;
- Grégoire Perra, enseignant et lanceur d’alerte sur les écoles Steiner-Waldorf et l’anthroposophie ;
- Sylvain Peterlongo, masseur-kinésithérapeute, membre du bureau du collectif No FakeMed ;
- Pr Nicolas Pinsault, vice-président du Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Dr Franck Ramus, CNRS ;
- Mathieu Repiquet, étudiant en médecine et en santé publique ;
- Pierre Rigal, secrétaire adjoint du Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Laurent Salsac, infirmier, membre du bureau du collectif No Fakemed ;
- Natalia Trouiller, lanceuse d’alerte sur les violences sexuelles dans l’Eglise catholique ;
- Stéphanie de Vanssay, enseignante, militante contre les dérives scolaires ;
- Brigitte Vincent, vice-présidente du Conseil national de l’ordre des masseurs kinésithérapeutes ;
- Dr Frederic Villebrun, médecin généraliste ;
- Dr Nicolas Winter, praticien hospitalier aux urgences pédiatriques Valenciennes et vulgarisateur sur les réseaux To be or not Toubib ;
- Dr Florian Zores, cardiologue.
Share this:
As recently as 2019, a quarter more homeopathic remedies were sold than today in Germany,reported the FRANKFURTER ALLGEMEINE ZEITUNG [my translation]. The largest manufacturer is removing individual remedies from its range and most state medical associations have cancelled the corresponding training courses for doctors.
Demand for homeopathic remedies continued to fall in 2024: while a good 45 million packs were sold in 2023, the number fell to around 43 million in 2024. The number of remedies dispensed on prescription fell even more sharply by 14 per cent from just under one million to just over 830,000.
According to the official pharmacy retail price, the total turnover of homeopathic remedies in 2024 was 779 million Euros. In 2019, sales were still around 834 million Euros, with around 56 million packs sold, a quarter more than last year.
This development is reflected in the companies’ figures. According to the annual report of the Willmar Schwabe Group, which includes Deutsche Homöopathie-Union (DHU), one of the largest manufacturers, sales in 2023 were negative in the ‘tense homeopathy environment’, some individual products had become unprofitable ‘and are being withdrawn from marketing’.
Homeopathy is repeatedly criticised due to the absence of active ingredients in the highly diluted remedies. Most state medical associations have cancelled corresponding additional training courses in recent years, including the medical association in Baden-Württemberg in 2024.
Just over a year ago, Federal Health Minister Karl Lauterbach announced plans to remove the possibility for health insurance companies to reimburse homeopathic and anthroposophic remedies as part of so-called statutory benefits. However, these plans have not yet been realized.
_________________________
A dismayed fan of homeopathy posted on ‘X’ [my translation]: “Homeopathy is on the retreat? Well, conventional medicine has successfully fought off the competition. They no longer want to share. They don’t care what happens to the patients.”
I don’t think this is quite true! What has happened is more simple and has little to do with competition. The evidence that homeopathy generates more good than harm is clearly not positive. Therefore – in the name of evidence, consumer protection, suffering patients and medical ethics – it is unavoidable that homeopathy is in decline. In fact, it seems surprising that it is still being reimbursed!
Share this:
On 27 January, the EXECUTIVE OFFICE OF THE PRESIDENTOFFICE OF MANAGEMENT AND BUDGETWASHINGTON, D.C. issued thisMEMORANDUM FOR HEADS OF EXECUTIVE DEPARTMENTS AND AGENCIES:
… Financial assistance should be dedicated to advancingAdministration priorities, focusing taxpayer dollars to advance a stronger and safer America,eliminating the financial burden of inflation for citizens, unleashing American energy andmanufacturing, ending “wokeness” and the weaponization of government, promoting efficiencyin government, and Making America Healthy Again. The use of Federal resources to advanceMarxist equity, transgenderism, and green new deal social engineering policies is a waste oftaxpayer dollars that does not improve the day-to-day lives of those we serve…
…each agency must complete a comprehensive analysis of all oftheir Federal financial assistance programs to identify programs, projects, and activities that maybe implicated by any of the President’s executive orders. In the interim, to the extent permissibleunder applicable law, Federal agenciesmust temporarily pauseall activities related toobligation or disbursement of all Federal financial assistance, and other relevant agency activitiesthat may be implicated by the executive orders, including, but not limited to, financial assistancefor foreign aid, nongovernmental organizations, DEI, woke gender ideology, and the green newdeal…
The memorandum effectively froze funding for research, and understandably sent shockwaves through the US science community. A federal judge in Washington temporarily blocked the order yesterday, but it had already caused panic. Many US universities already advised faculty members against spending federal grant dollars on travel, new research projects, equipment etc., and theNational Science Foundation canceled all of its grant review panels.
Some legal experts argue that Trump’s order is not legal: The US Constitution gives Congress, not the president, the power to appropriate funds. While lawyers are now trying to sort out the mess Trump created, scientists are spooked because, should Trump get away with his idiocy, the harm to science not just in the US but worldwide would simply be immeasurable.
Share this:
This study evaluated the real-world impact of acupuncture on analgesics and healthcare resource utilization among breast cancer survivors.
The authors selected from a United States (US) commercial claims database (25% random sample of IQVIA PharMetrics® Plus for Academics) 18–63 years old malignant breast cancer survivors who were experiencing pain and were ≥ 1 year removed from cancer diagnosis. Using the difference-in-difference technique, annualized changes in analgesics [prevalence, rates of short-term (< 30-day supply) and long-term (≥ 30-day supply) prescription fills] and healthcare resource utilization (healthcare costs, hospitalizations, and emergency department visits) were compared between acupuncture-treated and non-treated patients.
Among 495 (3%) acupuncture-treated patients (median age: 55 years, stage 4: 12%, average 2.5 years post cancer diagnosis), most had commercial health insurance (92%) and experiencing musculoskeletal pain (98%). Twenty-seven percent were receiving antidepressants and 3% completed ≥ 2 long-term prescription fills of opioids. Prevalence of opioid usage reduced from 29 to 19% (P < 0.001) and NSAID usage reduced from 21 to 14% (P = 0.001) post-acupuncture. The relative prevalence of opioid and NSAID use decreased by 20% (P < 0.05) and 19% (P = 0.07), respectively, in the acupuncture-treated group compared to non-treated patients (n = 16,129). However, the reductions were not statistically significant after adjustment for confounding. Patients receiving acupuncture for pain (n = 264, 53%) were found with a relative decrease by 47% and 49% (both P < 0.05) in short-term opioid and NSAID fills compared to those treated for other conditions. High-utilization patients (≥ 10 acupuncture sessions, n = 178, 36%) were observed with a significant reduction in total healthcare costs (P < 0.001) unlike low-utilization patients.
The authors concluded that,although adjusted results did not show that patients receiving acupuncture had better outcomes than non-treated patients, exploratory analyses revealed that patients treated specifically for pain used fewer analgesics and those with high acupuncture utilization incurred lower healthcare costs. Further studies are required to examine acupuncture effectiveness in real-world settings.
Oh, dear!
Which institutions support such nonsense?
- School of Pharmacy & Pharmaceutical Sciences, University of California Irvine, 802 W Peltason Dr, Irvine, CA, 92697-4625, USA.
- School of Pharmacy, Chapman University, RK 94-206, 9401 Jeronimo Road, Irvine, CA, 92618, USA.
- College of Korean Medicine, Kyung Hee University, Seoul, South Korea.
- Integrative Medicine Program, Departments of Supportive Care Medicine and Medical Oncology, City of Hope Comprehensive Cancer Center, Duarte, CA, USA.
- School of Pharmacy, Chapman University, RK 94-206, 9401 Jeronimo Road, Irvine, CA, 92618, USA.[email protected].
- School of Pharmacy & Pharmaceutical Sciences, University of California Irvine, 802 W Peltason Dr, Irvine, CA, 92697-4625, USA.[email protected].
And which journal is not ashamed to publish it?
It’s theBMC Med!
The conclusion is, of course, quite wrong.
Please let me try to formulate one that comes closer to what the study actually shows:
This study failed to show that a ‘real world impact’ of acupuncture exists. Since the authors were dissatisfied with a negative result, subsequent data dredging was undertaken until some findings emerged that were in line with their expectations. Sadly, no responsible scienctist will take this paper seriously.
Share this:
THE SUN (…yes, I know! …) reported last Sunday that figures from 20 trusts show they forked out for questionable treatments for more than 3,000 patients. Treatments also including acupuncture and aromatherapy cost a total of £269,000. If the figure is applied across all 120-plus trusts the true cost could be well over £1.5 million. Hull University Teaching Hospitals spent the most, at £170,000.
The Taxpayers’ Alliance, which did the analysis, said: “With long waiting lists, quack remedies cannot be allowed to divert precious resources.” Alternative medicine expert Dr Edzard Ernst said: “The NHS often uses complementary medicine rarely based on good evidence but on lobbying of proponents of quackery.”
End of quote
Whenever I am asked by journalists to provide a critical comment on so-called alternative medicine (SCAM), I have mixed feelings. On the one hand, I find it important to get a rational message out, particularly into certain papers. On the other hand, I dread what they might do with my comment, particularly certain papers. If I had £5 for every time I have been misquoted, I could probably buy a decent second-hand car! This is why I nowadays tend to give my comments in writing via e-mail.
To my relief, THE SUN quoted me (almost) correctly. Almost correctly, but not fully! Here is the question I was asked to respond to:NHS statistics show the health service spending more than £250,000 on complementary and alternative medicines last year. Do you think this is a sensible use of NHS funding? Are the benefits well proven enough to spend taxpayer money on these therapies?
And here is my attempt to respond in a concise way that SUN readers might still understand:
Complementary medicine is an umbrella term for more than 400 treatments and diagnostic techniques. Some of them work but many don’t; some are safe but many are not. If the NHS would spend £250000 – a tiny amount considering the overall expenditure in the NHS – on those few that do generate more good than harm, all might be fine. The problem, I think, is that the NHS currently uses complementary medicine rarely based on good evidence but often based on the lobbying of influential proponents of quackery.
As you see, it is good to deal with requests from journalists in writing!
Share this:
‘Chiropractic economics’ might be when chiropractors manipulate their bank accounts or tax returns, I thought. But, no, it is a publication! And a weird one at that – it evenpromotes the crazy idea of maintenance care:
The concept of chiropractic maintenance care has evolved significantly. Initially seen as a method for managing chronic pain, it now includes a broader range of patients and focuses on overall wellness.Modern maintenance care aims to keep patients healthy regardless of their symptoms or history, alleviating and preventing pain through regular, prolonged care. This approach is largely preventive, serving as both secondary and tertiary care. Studies show chiropractic maintenance care often includes diverse treatments such as manual therapy, stress management, nutrition advice and more, with flexible intervals typically around three months. This evolution underscores the importance of evidence-based, individualized patient care. This article shares the evolution of chiropractic maintenance care, looks at what a modern maintenance care appointment can include and explores best practices for DC maintenance care in 2024.
An interview study of Danish chiropractic care showed maintenance care sessions included a range of treatment modalities, including manual treatment and ordinary examinations alongside multiple packages of holistic additions, like stress management, diet, weight loss, advice on ergonomics, exercise and more. In other anecdotal accounts, chiropractic maintenance care seemed to follow a more traditional guideline of lower back pain management and adjustment. The study hypothesized that maintenance care could also help patients from a knowledge perspective, stating, “DCs could obviously play an important role here as ‘back pain coaches,’ as the long-term relationship would ensure knowledge of the patient and trust towards the DC.”
Researchers found that three-month intervals were the most common spacing of maintenance care treatments for patients. Most commonly, patients sought or scheduled chiropractic maintenance care over the course of one to three months.
Chiropractic maintenance care has evolved past simply being a method of ongoing chronic pain management. Today’s patients want to achieve overall wellness, and regular trips to their DC can become a part of that if you work to transition patients into a wellness plan after their acute phase of care is over.
_____________________________
The author of this article seems to have forgotten two little details:
- Chiropractic maintenance care is not supported by sound evidence, particularly in relation to economics (even the above cited paper stated: “We found no studies of cost-effectiveness of Maintenance Care”).
- Chiropractic maintenance only serves one economic purpose: it boosts the chiropractors’ income.
Yes, easy to forget, particularly if your name is ‘Chiropractic Economics’.
And also easy to forget that maintenance care would, of course, require informed consent. How would that look like?
Chiro (C) to patient (P):
If you agree, we will start a program that we call maintenance care.
P: Can you explain?
C: It consists of regular sessions of spinal manipulations.
P: That’s all?
C: No, I will also give you advice on keeping fit and living healthily.
P: Why do I need that?
C: It’s a bit like servicing your car so that it works reliably when you need it.
P: Is it proven to work?
C: Yes, of course, there are tons of evidence to show that a healthy life style is good for you.
P: I know, but I don’t need a chiro for that – what I meant do the manipulations keep my body healthy even if I have no symptoms?
C: The evidence is not really great.
P: And the risks?
C: Well, yes, if I’m honest, spinal manipulations can cause harm.
P: So, to be clear: you ask me to agree to a program that has no proven benefit and might cause harm?
C: I would not put it like that.
P: And how much would it cost?
C: Not much; just a couple of hundred per year.
P: Thanks – but no thanks.
Share this:
- Spinal Manipulation and Clinician-Supported Biopsychosocial Self-Management for Acute Back Pain
- More trouble for the Royal Family: Prince William’s charity has been reported to the Charity Commission of the UK
- The gradual loss of trust in homeopathy
- Hiring academics in different countries – similarities and differences
- Individualized Homeopathy for Pain of Calcaneal Spur?
- Deepak Chopra – Karma can be a real bitch!
- TCM herbal therapy for psoriasis?
- The Center for Inquiry (CFI) is raising alarm about new federal legislation of homeopathy
Note that comments can be edited for up to five minutes after they are first submitted but you must tick the box: “Save my name, email, and website in this browser for the next time I comment.”
The most recent comments from all posts can be seenhere.
- Talker onThe gradual loss of trust in homeopathy
- JK onThe gradual loss of trust in homeopathy
- Kurt Youngmann onSpinal Manipulation and Clinician-Supported Biopsychosocial Self-Management for Acute Back Pain
- Richard Rasker onThe gradual loss of trust in homeopathy
- Sundew onThe gradual loss of trust in homeopathy
- Richard Rasker onThe gradual loss of trust in homeopathy
- Edzard onThe gradual loss of trust in homeopathy
- Mutus Bellator onThe gradual loss of trust in homeopathy
- Talker onThe gradual loss of trust in homeopathy
- Sundew onThe gradual loss of trust in homeopathy
- February 2026 (12)
- January 2026 (26)
- December 2025 (25)
- November 2025 (25)
- October 2025 (28)
- September 2025 (26)
- August 2025 (26)
- July 2025 (27)
- June 2025 (27)
- May 2025 (29)
- April 2025 (28)
- March 2025 (26)
- February 2025 (25)
- January 2025 (27)
- December 2024 (25)
- November 2024 (26)
- October 2024 (27)
- September 2024 (24)
- August 2024 (27)
- July 2024 (28)
- June 2024 (27)
- May 2024 (28)
- April 2024 (27)
- March 2024 (26)
- February 2024 (28)
- January 2024 (31)
- December 2023 (29)
- November 2023 (30)
- October 2023 (28)
- September 2023 (26)
- August 2023 (30)
- July 2023 (28)
- June 2023 (26)
- May 2023 (28)
- April 2023 (25)
- March 2023 (31)
- February 2023 (27)
- January 2023 (29)
- December 2022 (26)
- November 2022 (26)
- October 2022 (26)
- September 2022 (27)
- August 2022 (29)
- July 2022 (26)
- June 2022 (28)
- May 2022 (26)
- April 2022 (27)
- March 2022 (29)
- February 2022 (26)
- January 2022 (27)
- December 2021 (27)
- November 2021 (28)
- October 2021 (28)
- September 2021 (27)
- August 2021 (29)
- July 2021 (30)
- June 2021 (28)
- May 2021 (30)
- April 2021 (27)
- March 2021 (27)
- February 2021 (24)
- January 2021 (27)
- December 2020 (27)
- November 2020 (25)
- October 2020 (28)
- September 2020 (26)
- August 2020 (28)
- July 2020 (28)
- June 2020 (27)
- May 2020 (28)
- April 2020 (29)
- March 2020 (31)
- February 2020 (26)
- January 2020 (27)
- December 2019 (24)
- November 2019 (26)
- October 2019 (26)
- September 2019 (25)
- August 2019 (26)
- July 2019 (27)
- June 2019 (25)
- May 2019 (30)
- April 2019 (25)
- March 2019 (24)
- February 2019 (25)
- January 2019 (28)
- December 2018 (27)
- November 2018 (27)
- October 2018 (26)
- September 2018 (25)
- August 2018 (27)
- July 2018 (28)
- June 2018 (28)
- May 2018 (28)
- April 2018 (26)
- March 2018 (30)
- February 2018 (25)
- January 2018 (30)
- December 2017 (16)
- November 2017 (18)
- October 2017 (20)
- September 2017 (16)
- August 2017 (17)
- July 2017 (16)
- June 2017 (20)
- May 2017 (29)
- April 2017 (27)
- March 2017 (22)
- February 2017 (19)
- January 2017 (26)
- December 2016 (24)
- November 2016 (19)
- October 2016 (26)
- September 2016 (23)
- August 2016 (21)
- July 2016 (24)
- June 2016 (21)
- May 2016 (28)
- April 2016 (20)
- March 2016 (20)
- February 2016 (16)
- January 2016 (16)
- December 2015 (15)
- November 2015 (18)
- October 2015 (19)
- September 2015 (14)
- August 2015 (18)
- July 2015 (20)
- June 2015 (22)
- May 2015 (19)
- April 2015 (15)
- March 2015 (14)
- February 2015 (15)
- January 2015 (21)
- December 2014 (18)
- November 2014 (21)
- October 2014 (22)
- September 2014 (13)
- August 2014 (21)
- July 2014 (12)
- June 2014 (18)
- May 2014 (21)
- April 2014 (7)
- March 2014 (11)
- February 2014 (10)
- January 2014 (17)
- December 2013 (14)
- November 2013 (19)
- October 2013 (22)
- September 2013 (26)
- August 2013 (15)
- July 2013 (11)
- June 2013 (18)
- May 2013 (11)
- April 2013 (12)
- March 2013 (10)
- February 2013 (16)
- January 2013 (12)
- December 2012 (9)
- November 2012 (9)
- October 2012 (7)
- "energy" healing
- acupressure
- acupuncture
- addiction
- ADHD
- aetiology
- AI
- Alexander Technique
- alternative medicine
- alternative therapist
- anthroposophical medicine
- antioxidants
- anxiety
- aromatherapy
- Arthritis Research UK
- asthma
- autism
- Ayurvedic medicine
- Bach Flower Remedies
- back pain
- BCA
- bias
- big pharma
- bogus claims
- bullshit
- Cancer
- caniosacral therapy
- case report
- case-control study
- causation
- charlatan
- children
- Chinese studies
- chiropractic
- clinical trial
- colonic irrigation
- commercial interests
- conflict of interest
- conspiracy
- COPD
- coronary heart disease
- cost-effectiveness
- cranial osteopathy
- critical thinking
- cult
- cupping
- death
- dentist
- depression
- detox
- diabetes
- diagnostic method
- diet
- doctors
- EBM
- economic evaluation
- eczema
- education
- Ernst's law
- essential oil
- evidence
- experience
- fallacy
- fatigue
- fish oil
- fraud
- gout
- Gua Sha
- guideline
- gullible consumer
- hay fever
- Healing Touch
- health insurance
- herbal medicine
- HIV
- holistic
- homeopathy
- hypercholesterolemia
- hypnotherapy
- IBS
- immunisation
- infant colic
- influenza
- informed consent
- insomnia
- integrated medicine
- integrative medicine
- iridology
- Iscador
- kinesiology
- King Charles
- leech therapy
- legal action
- lymph drainage
- lymph-oedema
- malpractice
- marijuana
- massage
- medical ethics
- menopause
- meta-analysis
- methodology
- Michael Dixon
- midwives
- migraine
- mountain sickness
- moxibustion
- multiple sclerosis
- musculoskeletal problems
- naturopathy
- nausea
- neck-pain
- neglect
- New Age
- NICE
- nurses
- obesity
- osteoarthritis
- osteopathy
- pain
- palliative care
- panacea
- patient choice
- pharmacists
- physiotherapists
- placebo
- plagiarism
- politics
- post-operative ileus
- pregnancy
- prevention
- Prince Charles
- probiotic
- proctophasia
- progress
- pseudo-science
- psoriasis
- quackery
- quality of life
- reflexology
- regulation
- Reiki
- religion
- research
- reviewer bias
- rheumatoid arthritis
- risk
- risk/benefit
- Samueli Institute
- satire
- scientific misconduct
- shoulder-pain
- Simon Singh
- slimming aids
- smoking cessation
- social prescribing
- spinal manipulation
- study design
- supplements
- survey
- symptom-relief
- systematic review
- tai chi
- TCM
- test of time
- Therapeutic Touch
- Uncategorized
- urin therapy
- vaccination
- veterinary medicine
- vitamin
- wellness
- WHO
- yoga